Enteral nutrition is beneficial
Guidelines recommend to start enteral feeding early, within 24–48 hours1-3, once haemo-dynamically stable.
Enteral feeding:
- Promotes the structural integrity of the gut by maintaining tight junctions between intraepithelial cells4-6
- Stimulates gastrointestinal blood flow4-6
- Sustains the immune response by gut-associated lymphoid tissue (GALT)4-6, which in turn supports mucosal-associated lymphoid tissue (MALT) in lung, liver and kidneys. This may lower the risk of multiorgan failure4-6
- Preserves lean body mass and muscle function, which are particularly important for the outcome of critically ill patients7-9
Starting enteral feeding early
in critically ill patients helps to achieve nutritional targets quickly to avoid energy and protein deficits.
In addition, it provides a wide range of other important benefits:
Clinical benefits of EARLY enteral feeding:
+ Significantly reduces infectious complications1-3
+ May reduce length of hospital stay10
+ Significantly reduces mortality1,11
Early protein provision matters
Early enteral protein supply, especially in the acute phase, may be beneficial in terms of protein metabolism12. Critically ill patients lose up to 20% of skeletal muscle mass during the first 10 days on ICU13. Providing 1.1-1.5 g protein per kg of fat-free mass per day has been shown to reduce protein catabolism by 50% over a 10-day period soon after ICU admission14.

Protein is the most important macro-nutrient for:
- Wound healing
- Immune function
- Conservation of lean body mass
Please consider
In acute critical illness, protein needs are higher than energy requirements and they cannot easily be met by providing standard enteral formulae1.
In addition, patients in the acute phase often receive calories from other sources, including glucose-containing fluids and lipid-based medications15.
Nutrition support for ICU patients according to the ESPEN 2018 guideline
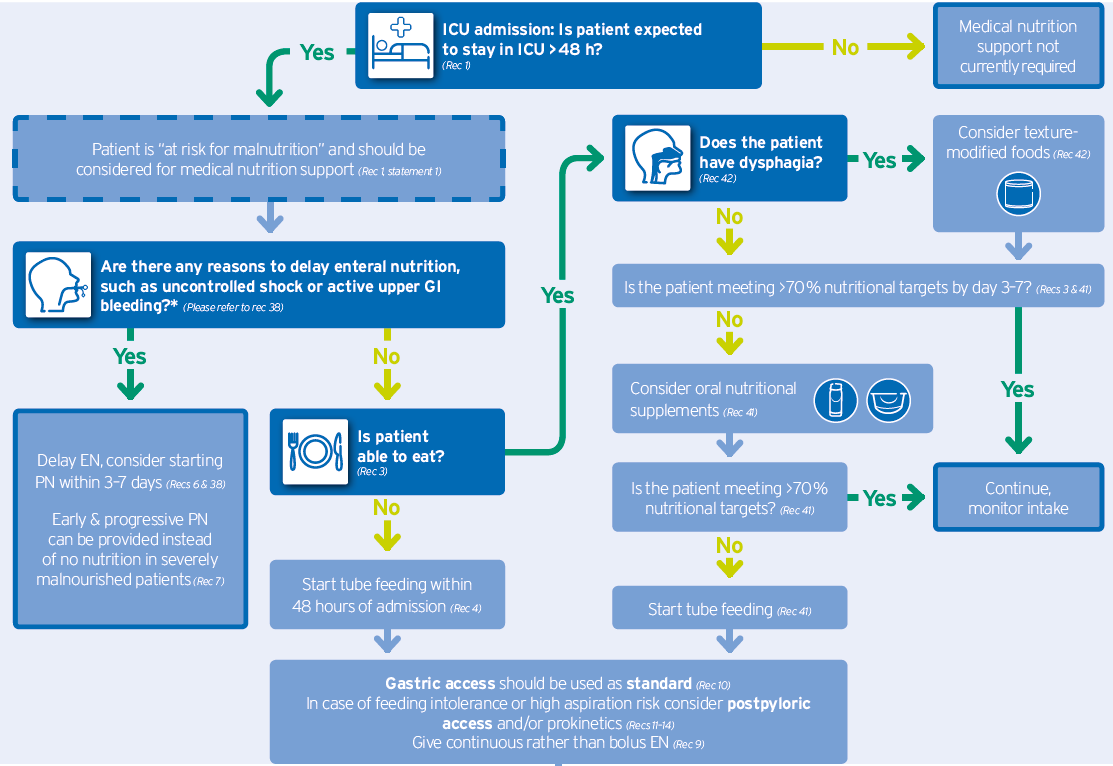
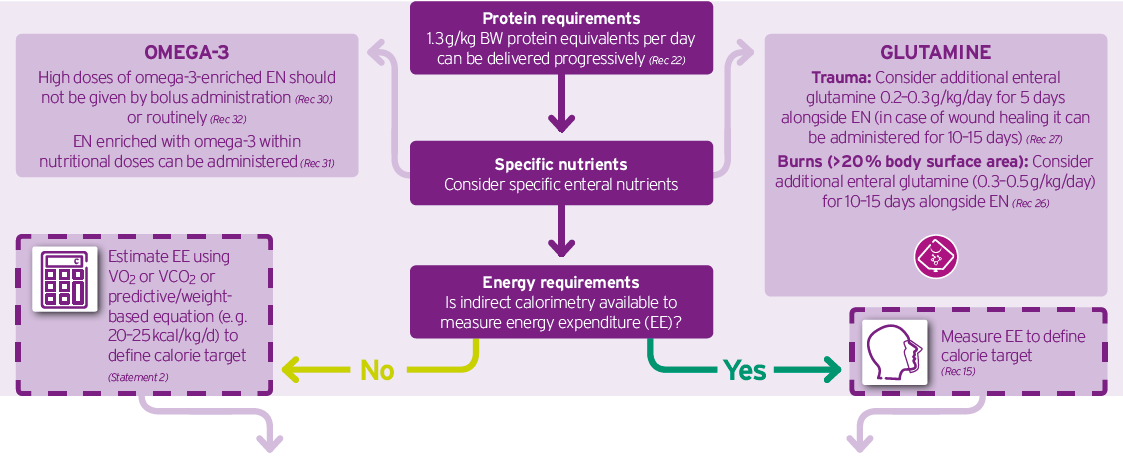

Decision tree Nutrition in the ICU.pdf
Download the complete decision tree according to ESPEN ICU guidelines 2018 here.
- Filename
- Decision tree Nutrition in the ICU.pdf
- Size
- 467 KB
- Format
Recommendations for nutrition support in Intensive Care
Early acute phase
Recommendations of ASPEN1 and ESPEN2
- Protein intake in the range of 1.2–2.0 g/kg BW/day (may be even higher in burn, multitrauma or obese patients)1
- Hypocaloric nutrition (<70% energy needs) in the early phase of acute illness up to the first week of ICU stay*2
- Start enteral feeding early within 24–48 hours1, 2
*If predictive equations are used to estimate the energy need, hypocaloric nutrition (below 70 % estimated needs) should be preferred over isocaloric nutrition for the first week of ICU stay.

Fresubin Intensive
meets the current recommendations:
- 1.2 kcal/ml tube feed
- 10 g/100 ml protein:
100 % whey hydrolysate rich in the branched chain amino acid leucine
Recovery phase
Fresubin 2 kcal HP or Fresubin 2 kcal HP Fibre
- High protein and high energy tube feed with or without fibre
- For periods of high energy and protein needs (> 1.3 g protein / kg body weight)

Oral Nutritional Supplements
References:
1. McClave SA, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN. 2016; 40(2):159–211.
2. Singer P, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48-79.
3. Reintam Blaser A, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med 2017 (epub ahead of print).
4. Kang W, Kudsk KA. Is there evidence that the gut contributes to mucosal immunity in humans? JPEN. 2007; 31(3):246–58.
5. Kudsk KA. Current aspects of mucosal immunology and its influence by nutrition. Am J Surg 2002; 183(4):390–8.
6. Jabbar A, et al. Gut immunology and the differential response to feeding and starvation. Nutr. Clin. Pract. 2003; 18(6):461–82.
7. Lee ZY, et al. Enhanced Protein-Energy Provision via the Enteral Route in Critically Ill Patients (PEP uP Protocol): A Review of Evidence. Nutr. Clin. Pract. 2016; 31(1):68–79.
8. McClave SA, et al. Feeding the critically ill patient. Crit Care Med 2014; 42(12):2600–10.
9. Berger MM, Pichard C. Development and current use of paren-teral nutrition in critical care - an opinion paper. Crit Care 2014; 18(4):478.
10. Marik PE, Zaloga GP. Early enter-al nutrition in acutely ill patients: A systematic review. Crit Care Med 2001; 29(12):2264–70.
11. Tian F et al. Early Enteral Nutrition Provided Within 24 Hours of ICU Admission: A Meta-Analysis of Randomized Controlled Trials. Crit Care Med. 2018;46(7):1049-1056.
12. Liebau F, et al. Effect of initiating enteral protein feeding on whole-body protein turnover in critically ill patients. Am J Clin Nutr 2015; 101(3):549–57.
13. Puthucheary ZA, et al. Acute skeletal muscle wasting in critical illness. JAMA 2013; 310(15):1591–600.
14. Singer P, et al. Pragmatic approach to nutrtition in the ICU: Expert opinion regarding which calorie protein target. Clin Nutr 2014;33:246-51.
15. Bousie E, et al. Relevance of non-nutrition-al calories in mechanically ventilated critically ill patients. Eur J Clin Nutr 2016; 70(12):1443–50.



